|
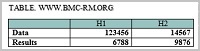
CONTENTS COMPLIANCE WITH ETHICAL STANTARDS Table 1Clinical characteristics of patients according to NYHA class. Table 2Chronic medications and outcomes. Table 3. Readings of the CHF patients according to NYHA groups. Table 5Correlation of drug usage with PLT, MPV and fibrinogen concentration (n=203). |
Does Platelet and Inflammatory Readings Differ between Chronic Heart Failure Patients‘ Groups According to NYHA Functional Classes? 1Department of Biochemistry, Lithuanian University of Health Sciences, Keywords: platelet aggregation; mean platelet volume; heart failure; C-reactive protein (CRP); fibrinogen DOI: 10.18097/BMCRM00111 INTRODUCTION
Reduced heart function has been determined to be an independent risk factor for venous thromboembolism (VTE) [1]. Thrombotic complications occur in 11 – 44% of chronic heart failure (CHF) patients. The incidence of VTE in heart failure patients was found the highest in patients classified as NYHA IV (NYHA II: 4.4%, NYHA III: 4.8%, NYHA IV: 25.5%, p < 0.01) [2]. VTE in patients with heart failure varies from no risk to high risk (2.9 – 32.4 %) [3]. Postmortem studies in heart failure patients shewed an incidence of pulmonary thromboembolism of ≤ 32% [4]. Increased platelet activation in CHF patients may contribute to thrombogenesis [5]. Mean platelet volume (MPV) can be an indicator of platelet activation. The studies have shown that the large platelets are more active [6]. Increased MPV values correlate with clinical status of patients with acute heart failure [7]. Some authors suggested that MPV correlated with platelet function and activation [8]. Several studies shewed that MPV did not [9]. Fibrinogen concentration in plasma strongly correlates with blood viscosity. Increasing of plasma viscosity increased thrombotic affinity [10]. C-reactive protein (CRP) concentration was shown to be significantly higher in patients after myocardial infarction with heart failure in comparison without heart failure [11]. CRP was found to be higher in the worse condition heart failure patients with reduced or preserved ejection fraction (EF) [12, 13]. There is no information in the literature about the difference of the MPV in different condition of CHF patients according to NYHA functional classes. Moreover, it was shown, that MPV depended on the measurement time from the venipuncture and would be done within results 120 min after venipuncture, using ethylendiamintetraacetic acid (EDTA) [14]. The aims of this study were 1) to test the hypothesis that prothrombotic state depends on inflammation, 2) to verify, if MPV correlate with platelet aggregation. We have compared the inflammation markers (fibrinogen concentration, CRP) and platelet readings (platelet count, MPV and platelet aggregation) in CHF patients groups according to NYHA and evaluated the correlation between the platelet and inflammatory readings. Comparison of platelet and inflammation readings between chronic heart failure (CHF) patient groups according to NYHA functional classes can help to prove or reject the hypothesis. The confirmed hypothesis would allow to use anti-inflammatory drugs to reduce or avoid thrombosis in CHF patients and to use MPV as marker of platelet activity. MATERIALS AND METHODS Subjects Patients, admitted to the Department of Cardiology, Hospital of Lithuanian University of Health Sciences, during the period , 01.01.2016 – 01.03.2018 and diagnosed with CHF were screened for inclusion in the study. 203 CHF patients with reduced ejection fraction (systolic heart failure class I‒IV according to NYHA (New York Heart Association)), who had not been using any antiaggregants during the last two weeks and experienced no other factors affecting platelet and gave written informed consent to participate, with stable clinical state were included in the study. Patients with renal failure (eGFR < 90 ml/min.), acute and chronic infection, acute coronary syndromes, or connective tissue disease and consuming platelet affecting agents were excluded from the study (n = 153). The diagnosis of CHF was made and NYHA functional class was established following the guidelines for the diagnostics and treatment of heart failure approved by the European Society of Cardiology [15] at the time of hospitalization. The clinical state was considered stable provided that there were no changes in functional class according to NYHA, medications used during the past 3 – 4 weeks, there were no new heart failure symptoms. Table 1 shows the characteristics of the different NYHA class patients. Table 2 shows chronic medications and outcomes.
Methods The heart echocardiography (TEE) and 6 min. walking test were performed, complete blood count, fibrinogen, CRP, NT-pro-BNP concentrations and platelet aggregation were determined. Blood samples for the complete blood count testing were taken from the forearm vein with a 20-G needle into 4.5-mL vacuum tubes with EDTA and were put into haematological analyser COULTER LH 780 («Beckman Coulter», USA). In order to investigate platelet aggregation, blood samples were taken from the forearm vein into 5-mL vacuum tubes with 3.8% sodium citrate. In order to prepare platelet rich plasma, the blood was centrifuged at 100 g for 15 min at room temperature. Platelet poor plasma was obtained when the rest of blood was centrifuged at 1000 g for 30 min. Platelet aggregation was investigated in platelet rich plasma using the aggregometer («Chrono-Log», USA) by the standard Born method [16]. ADP (3.8 mM and adrenalin (ADR, 4.5 mM) (the final working concentration), Chrono-log P/N 384) were used for aggregation induction. NT-pro-BNP level was measured by immune-electro-chemo-luminescent assay on Elecsys 1010 analyzer («Roche», Germany, sets produced by «R&D Systems», USA). CRP level was measured using immunonefelometry («Dade Behring», Germany). Fibrinogen concentration was investigated by the Clauss method (STACompact Max and reagents STA Fibrinogen, «Diagnostika Stago», USA). Statistics For the statistical analysis, we used the Statistical Package for the Social Sciences (IBM SPSS 20). Normal distribution was assessed using the Shapiro (when n < 50) and Kolmogorov-Smirnov (when n > 50) tests. Categorical variables were defined as a percentage, and comparisons were made using the chi-square test. Quantitative variables nonparametric distributed were expressed as median and min-max values. Quantitative variables parametric distributed were expressed as mean ± SD, and, for the comparison of variables between the groups, ANOVA (for variables parametric distributed) and Welch’s test (for the parameters showing the nonparametric distribution and to compare more than two groups with different count of variables) were used. The results were assessed using post-hoc analysis. Spearman’s correlation analysis was performed. Differences were considered as statistically significant at p < 0.05. RESULTS The study population consisted of 203 patients with CHF (32 with NYHA I functional class, (16%), 78 with NYHA II functional class (38%), 62 with NYHA III functional class (31%) and 31 with NYHA IV functional class (15%). The patients in NYHA III and NYHA IV groups were statistically significant older than NYHA I patients (Table 1). BMI was statistically higher in NYHA I than in NYHA IV patients. SBP and DBP were also higher in NYHA I group than in NYHA IV. There were no statistically significant differences in current medications usage and outcomes between the groups (Table 2). Laboratory and other readings of patients subdivided into groups according to NYHA class are presented in Table 3. There were no statistically significant differences in platelet count between the groups. The MPV was significantly higher in NYHA IV group than in NYHA III, NYHA II and NYHA I groups. There were no statistically significant differences in platelet aggregation. There were no statistically significant differences in fibrinogen concentration and CRP. NT-pro BNP concentration gradually increased from NYHA I to NYHA IV group. Data from the all patients were pooled to analyze the correlation between PLT, MPV, fibrinogen concentration and other investigated parameters. There was a weak correlation between the PLT and CRP (r = 0.293, p = 0.01, Table4). MPV correlated with fibrinogen concentration (r = 0.205, p = 0.012), with age (r = 0.277, p = 0.001), with NYHA functional class (r = 0.368, p = 0.001) and LFEF (r = 0.206, p = 0.031, not shown in the table 4). It was found, that PLT weakly correlated with statins usage (r = 0.158, p = 0.046) and fibrinogen concentration correlated with nitrates usage (r = 0.246, p < 0.001, Table 5). MPV weakly correlated with some drugs usage: statins (r = -0.148, p = 0.048), digoxin (r = 0.191, p = 0.011), heparin (r = 0.242, p = 0.001), and calcium channel blockers (r = 0.277, p < 0.001).
DISCUSSION Considering literature data, that VTE is highest in patients classified as NYHA IV [2], we hoped to find the higher values MPV, platelet aggregation, fibrinogen concentration and CRP concentration in groups of CHF patients of higher NYHA functional class. To avoid the influence of preanalytical conditions on the MPV result, all the blood samples were investigated strictly within 120 min after venipuncture. It was found that only the MPV demonstrated statistically significant increase according to NYHA (Table 3). The bigger platelet is supposed to be more active [6]. It has been demonstrated that MPV increased in decompensated HF and correlated with disease severity in acute HF patients [17]. Chronic hypoxia has been shown to stimulate cytokine mediated production of large platelets from the bone marrow [18]. Our results confirms that in worse CHF condition MPV is higher. This finding is sustained by another finding, that there was a moderate correlation between the MPV and NYHA. It is in accordance with other research findings. They sustain the bigger MPV in many cardiovascular pathologies [6] that may lead to thrombosis. Our findings that MPV correlated with the age and that the patients with NYHA III and IV functional class were older than those with NYHA I and II, might raise some doubt. MPV correlation with LVEF takes place thus supporting the relationship between MPV and thrombosis. As it is stated in the literature, lifestyle, antihypertensive, lipid-lowering and diet therapies can affect MPV values [19]. We found a weak correlation between MPV and statins, digoxin, heparin, thyroxine and calcium channel blockers usage. Some authors have found that statins significantly decreased the MPV [20]. There was no significant difference between drugs usage in all our investigated groups. This suggest that the MPV increas according to NYHA groups obviously depend on patient's condition, but not on the drugs usage. Some researches revealed significant correlations between MPV and aggregation levels in healthy donors [21] and concluded that the MPV represented platelet activity [22]. Therefore we hoped to find the rising platelet aggregation according to NYHA class. But our results did not show the statistically significant increase. Also we did not find correlation between MPV and platelet aggregation. Puurunen at al. [23] reported that platelet aggregation was only weakly associated with VTE. De Luca et al. [9] did not observe any significant relationship between MPV and platelet aggregation. Levels of glycoprotein IIb-IIIa and Ib and P-selectin were higher in patients with acute condition than in healthy persons [21]. In contrast to our expectations, we did not found any correlation between MPV and platelet aggregation; however we did find a weak correlation between MPV and fibrinogen concentration. This is consistent with literature findings, were MPV is pshown to be related to the inflammatory condition [19]. It is still unclear whether PLT serves as a marker of HF worsening [24, 25]. With regard to these findings we aimed to compare the PLT in CHF groups according to NYHA class. The PLT difference between CHF patients in NYHA groups was not found. Our finding, that PLT weakly correlates with CRP, may confirm, that low inflammation can be related to PLT. It is in accordance with the authors stating the platelets are important coordinators of inflammation and both innate and adaptive immune responses [26]. Pro- or anti-inflammatory behavior of platelets is highly dependent on cause of inflammation, which defines the pathways and extent of leukocyte, platelet and endothelial activation [27]. Therefore the PLT significance in thrombosis should be clarified in more extensive studies. Plasma fibrinogen concentration strongly correlates with plasma viscosity. Plasma viscosity increases the shear stress, which promotes platelet activation [5, 28]. We have proposed the following our hypothesis: the worse CHF patients’ condition (NYHA functional class) is, the higher fibrinogen concentration should be. However we didn't find statistically significantly increasing of plasma fibrinogen concentration according to NYHA class. Medians increased according to NYHA groups, but did not reach the level of statistical significance. There was no correlation between platelet aggregation and PLT. Increased levels of CRP have been shown to predict adverse outcomes in patients with reduced and preserved ejection fraction [28]. Elevated CRP levels have been shown to correlate with worse cardiac function too [29]. CRP takes place in activation of the complement pathway and release of proinflammatory cytokines, it induces the tissue factor expression in monocytes and leads to the prothrombotic state [11]. Li el al. revealed significantly higher CRP in CHF patients with reduced EF [13]. Therefore we aimed to compare CRP concentration in CHF patients with reduced EF groups according to NYHA class. But we did not find any significant differences between the groups, when the CRP median was the highest in NYHA IV class. The CRP correlation with fibrinogen concentration is logical, because both are inflammatory proteins, and fibrinogen regulation pathways are related to inflammation: activated monocytes produce cytokines, and cytokines induce the synthesis of fibrinogen [30]. In summary, MPV rising in the patients’ groups and correlation between MPV and NYHA class, and plasma fibrinogen concentration, correlation between PLT and CRP, correlation between CRP and NT-proBNP concentration confirm, that low inflammation can take place in the MPV rising. We have not found the correlation between the platelet aggregation and MPV, so the relationship between the platelet activity and MPV in the CHF patients’ needs to be clarified. According to our information, this is the first work in which MPV, PLT, CRP and fibrinogen concentrations have been evaluated in CHF patients according to NYHA functional class. Our study had some limitations. One of them was the small sample size. The second one was, that we did not measure the level of inflammatory markers, such as TNF-α, IL-6, and platelet activation markers (P-selectin, CD40, glycoprotein IIb/IIIa, Ib, PTX3 and others). This was an observational and nonrandomized study. Therefore it can be considered as a prototype of further prospective and randomized studies to compare the correlation of the MPV and platelet aggregation, LFEF, inflammatory readings, age and others. CONCLUSIONS
MPV statistically significant increases according to NYHA functional class. There was no difference in PLT, platelet aggregation, fibrinogen and CRP concentrations in the CHF groups according to NYHA. PLT correlated with CRP, MPV correlated with NYHA functional class and plasma fibrinogen concentration, NT-proBNP concentration correlated with CRP.
COMPLIANCE WITH ETHICAL STANTARDS All the investigations were approved and conducted in accordance with the guidelines of the local Bioethics Committee and adhered to the principles of the Declaration of Helsinki and Title 45, U.S. Code of Federal Regulations, Part 46, Protection of Human Subjects (revised November 13, 2001, effective December 13, 2001). The subjects gave informed consent. The study was approved by the Regional Bioethics Committee at the Lithuanian University of Health Sciences (No. BE-2-102). FUNDING This work was supported by the Lithuanian university of health sciences. REFERENCES
|