Detection of SARS-Cov-2 N-Protein in Mesenchymal Cells of Umbilical Warton's Jelly in WOMEN with COVID-19
1Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, 4 bld. 2 Oparina str., Moscow, 117513 Russia; *email: vfrankevich@gmail.com
2Academician A.P. Avtsyn Research Institute of Human Morphology, Moscow, Russia
Keywords: SARS-Cov-2; placenta; umbilical cord; fibroblast-like cells; Wharton's jelly
DOI:10.18097/BMCRM00165
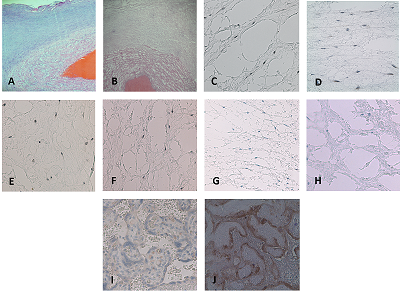
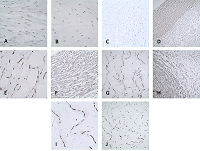
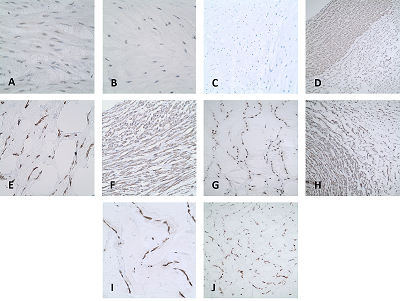
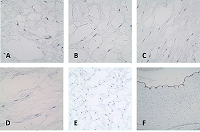
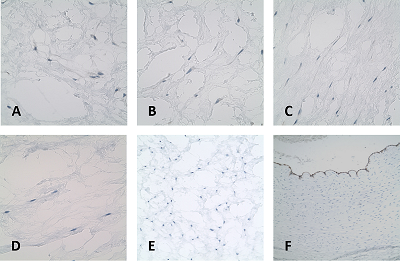
Despite the large number of studies on the new coronаvirus infection SARS-Cov-2 characterized by vascular damage on the impact of the virus on the mother-placenta-fetus system remains unknown. The umbilical cord, according to its functional purpose, is a complex of vessels protected from external influences by the embryonic connective tissue –Wharton's jelly. The aim of the study was to detect the structural components of SARS-Cov-2 in the histological structures of umbilicals cord in patients with COVID-19 in the tissues of the umbilical cord of women with COVID-19. The main group included 40 pregnant women who were treated at the academician V. I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology (March-April 2020) with a confirmed diagnosis of COVID-19 (according to the positive PCR test of a nasopharyngeal swab) and 40 pregnant women of the comparison group, without clinical symptoms and laboratory tests, including the negative PCR test. As a result of the immunohistochemical study of the umbilical cord with primary antibodies to the SARS-CoV-2 N-protein in the COVID-19 group, staining of the cytoplasm of fibroblast-like cells and single macrophages Wharton's jelly was detected (p<0.05). In the group of women without coronavirus infection no staining in Wharton's jelly cells was detected. The probable persistence of viral particles in mesenchymal cells and macrophages of the Wharton's jelly in the umbilical cord can be important for establishment new aspects of influence СOVID-19 on the mother-placenta-fetus system. Our results suggesting persistence of COVID-19 viral proteins in mesenchymal cells of the umbilical cord could be an important in establishing new pathogenic mechanisms for the fetal protection against viruses.
|
CLOSE
|
Table 1.
Clinical characteristics of pregnant women included in the study and newborns.
|
FUNDING
This work was supported by the Russian Foundation for Basic Research (project no. 20–015–00104).
REFERENCES
- Kovrigina, A.M., Shalamova, E.A., Berezovskij, Iy. S., (2020). Patomorfologicheskaya i immunogistoximicheskaya xarakteristika izmenenij limfaticheskix uzlov u umershix ot covid-19 po dannym autopsij. Klinicheskaya i Eksperimental'naya Morfologiya., 9(4), 12–23. DOI
- Atala, A., Henn, A., Lundberg, M. (2020). Regen med therapeutic opportunities for fighting COVID-19. Stem Cells Translational Med., 1, 5–13. DOI
- Becker, R.C. (2020). COVID-19-associated vasculitis and vasculopathy. J. Thromb Thrombolysis., 50(3), 499-511. DOI
- Lang, M., Som, A., Carey, D., et al. (2020). Pulmonary vascular manifestations of COVID-19 pneumonia. Radiol Cardiothorac Imaging., 2(3), e200277. DOI
- McGonagle, D., Bridgewood, C., Ramanan A.V., et al. (2021). COVID-19 vasculitis and novel vasculitis mimics. Lancet Rheumatol., 3(3), e224-e233. DOI
- Morris, D., Patel, K., Rahimi, O., et al. (2021). ANCA vasculitis: A manifestation of Post-Covid-19 Syndrome. Respir Med. Case Rep., 34, 101549. DOI
- Baergen, R. N. (2022). Benirschke’s Pathology of the Human Placenta. Springer Nature, 954 p.
- Lanzoni, G., Linetsky, E., Correa, D., et al. (2020). Umbilical Cord-derived Mesenchymal Stem Cells for COVID-19 Patients with Acute Respiratory Distress Syndrome (ARDS). Cell R4 Repair Replace Regen Reprogram., 8, e2839. DOI
- Paladino, F.V., Rodrigues, J.M., Silva, A., Goldberg, A. C. (2019). The immunomodulatory potential of wharton's jelly mesenchymal stem/stromal cells. Stem Cells Int., 3548917. DOI
- Alanazi, A., (2021) COVID-19 and the role of stem cells. Regen Ther., 18, 334- 338. DOI
- Babal, P., Krivosikova, L., Sarvaicova, L., et al. (2021) Intrauterine fetal demise after uncomplicated COVID-19: What can we learn from the case? Viruses, 13(12), 2545. DOI
- Biringer, K., Sivakova, J., Marcinek, J., et al. (2021) Placental pathology concerning sudden fetal demise in SARS-CoV-2 positive asymptomatic pregnant female. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub., 165, 328-331. DOI
- Lesieur, E., Torrents, J., Fina, F., et al. (2021). Congenital infection of SARS- CoV-2 with intrauterine foetal death: a clinicopathological study with molecular analysis. Clin. Infect. Dis., ciab840. DOI
- Libbrecht, S., Van Cleemput, J., Vandekerckhove, L., et al. (2021) A rare but devastating cause of twin loss in a near-term pregnancy highlighting the features of severe SARS-CoV-2 placentitis. Histopathology, 79(4), 674-676. DOI
- Marinho, P.S., Cunha, A., Chimelli, L., et al. (2021) SARS-CoV-2 mother-to- child transmission and fetal death associated with severe placental thromboembolism. Front Med (Lausanne), 16(8), 677001. DOI
- Schwartz, D.A., Graham, A.L. (2020) Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses, 12(2), 194. DOI
- Vacchi, C., Meschiari, M., Milic, J., et al. (2020) COVID-19-associated vasculitis and thrombotic complications: from pathological findings to multidisciplinary discussion. Rheumatology (Oxford), 59(12), e147-e150. DOI
- Nizyaeva, N.V., Lomova, N.A., Dolgopolova, E.L,i dr. (2021) Vliyanie novoj koronavirusnoj infekcii COVID-19 na sistemu «mat'–placenta– plod». Vestnik RGMU, 2021(2), 27–34. DOI
- Gioia, C., Zullo, F., Vecchio, R. C., et al. (2022) Stillbirth and fetal capillary infection by SARS-CoV-2 632 Am. J. Obstet. Gynecol. MFM, 4(1), 100523. DOI
- Garrido-Pontnou, M., Navarro, A., Camacho, J., et al. (2021) Diffuse trophoblast damage is the hallmark of SARS-CoV-2-associ-ated fetal demise. Mod. Pathol., 34, 1704-1709. DOI
- Marton, T., Hargitai, B., et al. (2021) Massive perivillous fibrin deposition and chronic histiocytic intervillositis a complication of SARS-CoV-2 Infection. Pediatr. Dev. Pathol., 24, 450-454. DOI
- Hosier, H., Farhadian, S. F., Morotti, R. A., at al. (2020) SARS–CoV-2 infection of the placenta. J. Clin. Invest., 130(9), 4947-4953. DOI
- Nagamatsu, T., Schust D. J. (2010) The immunomodulatory roles of macrophages at the maternal-fetal interface. Reprod. Sci., 17(3), 209-218. DOI
- Gurevich P.S. (2011) Immunopatologiya zarodyshevogo, `embrional'nogo i rannego fetal'nogo periodov cheloveka. Allogennye konflikty, Izrail', 182 p.
- Liu, W., Li, J. (2021) The SARS-CoV-2 nucleocapsid protein and its role in viral structure, biological functions, and a potential target for drug or vaccine mitigation. Viruses, 13(6), 1115. DOI
- Singh, D., Yi, S.V. (2021) On the origin and evolution of SARS-CoV-2. Exp. Mol. Med., 53, 537–547. DOI:10.1038/s12276-021-00604-z
- Uribe-Querol, E., Rosales, C. (2020) Phagocytosis: Our Current Understanding of a Universal Biological Process. Front Immunol., 11, 1066. DOI
- Beyerstedt, S., Casaro, E. B., Rangel, É. B. (2021) COVID-19: angiotensin- converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur. J. Clin. Microbiol. Infect. Dis., 40(5), 905-919. DOI
- Yang, J., Petitjean, S. J. L., Koehler, M., et al. (2021) Molecular interaction and inhibition of SARS-CoV-2 binding to the ACE2 receptor. Nat. Commun., 11(1), 4541. DOI
- Sukhacheva, T.V., Nizyaeva, N.V., Samsonova, M.V., et al. (2021) Morpho- functional changes of cardiac telocytes in isolated atrial amyloidosis in patients with atrial fibrillation. Sci Rep., 11, 3563. DOI
- Adukia, S. A., Ruhatiya, R. S., Maheshwarappa, H. M., et al. (2020) Extrapulmonary features of COVID-19: A Concise Review. Indian J. Crit. Care. Med., 24(7), 575-580. DOI:10.5005/jp-journals-10071-23476
- Elrobaal, I. H., New, K. J. (2021) COVID-19: Pulmonary and extra pulmonary manifestations. Front. Public Health, 9, 711616. DOI
- Gupta, A., Madhavan, M.V., Sehgal, K., et al. (2020) Extrapulmonary manifestations of COVID-19. Nat. Med., 26, 1017–1032. DOI
- Nasonov, E.L., Lila, A.M., Mazurov, V.I., et al. (2021) Coronavirus disease 2019 (COVID-19) and immune-mediated rheumatic diseases. recommendations of the association of rheumatologists of russia. rheumatology Science and Practice., 59(3), 239-254. DOI DOI