MMP-9, MMP-2, VEGF and VEGFR-2 as Factors of Invasion and Angiogenesis in Squamous Cell Carcinoma of the Cervix
Institute of Biomedical Chemistry, Pogodinskaya Street, 10, Moscow 119121, Russia; *e-mail: ryzhakova.olga@list.ru
Keywords: ММP-2; ММP-9; VEGF; VEGF receptor; tumor progression; squamous cell carcinoma of the cervix
DOI:10.18097/BMCRM00187
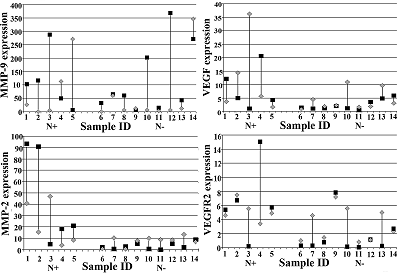
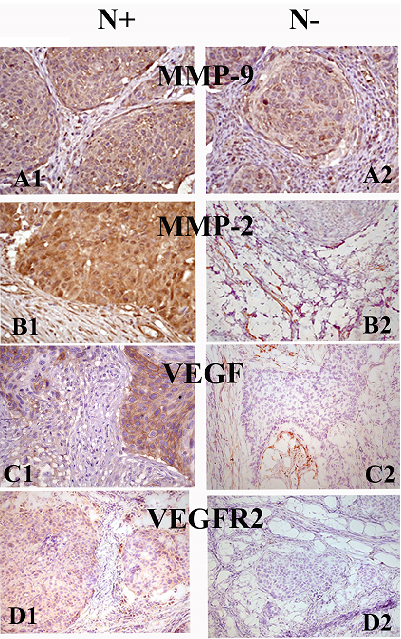
Tissue destruction and angiogenesis play an important role in malignant tumor progression. They are responsible for the tumor growth and progress and its ability to invade and metastasize. The key role in the destructive processes belongs to matrix metalloproteinases (MMPs), which are able to cleave almost all components of the extracellular matrix (ECM). Gelatinases MMP-2 and MMP-9 hydrolyze type IV collagen, the main component of basement membranes, thereby releasing various biologically active molecules from ECM, including vascular endothelial growth factor (VEGF). VEGF is a key regulator of angiogenesis. The main mediator of the biological action of VEGF is its receptor VEGFR2. This study was aimed at assessing the relationship between the expression of the main factors of tissue destruction and angiogenesis - MMP-2, MMP-9, VEGF and VEGFR2 in the early and later stages of cervical squamous cell carcinoma (CSCC). The work was performed using samples of tumor and surrounding morphologically normal tissue, obtained from patients with or without metastases to regional lymph nodes. We have shown that MMP-9 is significantly expressed in tumors in CSCC already at the early stages of tumor progression. At later stages of the disease (when metastases to regional lymph nodes are detected in patients), the expression of MMP-2, VEGF and VEGFR2 increases markedly both in the tumor and in the morphologically normal tissue surrounding the tumor and makes an additional contribution to the processes of destruction, angiogenesis and metastasis. We assume that MMP-2, VEGF and VEGFR2 can be considered as negative markers of the course of CSCC.
|
CLOSE
|
Table 1.
Characteristics of clinical material. Data obtained from patients medical history.
|
|
CLOSE
|
Table 2.
Primers sequence used in the work.
|
FUNDING
The work was performed within the framework of the Program for Basic Research in the Russian Federation for a long-term period (2021-2030) (№ 122022800499-5).
REFERENCES
- Wyganowska-Świątkowska, M., Tarnowski, M., Murtagh, D., Skrzypczak-Jankun, E., Jankun, J. (2019) Proteolysis is the most fundamental property of malignancy and its inhibition may be used therapeutically (Review). Int. J. Mol. Med., 43(1), 15-25. DOI
- Cabral-Pacheco, G.A., Garza-Veloz, I., Castruita-De la Rosa, C., Ramirez-Acuña, J.M., Perez-Romero, B.A., Guerrero-Rodriguez, J.F., Martinez-Avil, N., Martinez-Fierro, M.L. (2020) The roles of matrix metalloproteinases and their Inhibitors in human diseases. Int. J. Mol. Sci., 21(24), 9739. DOI
- Kapoor, C., Vaidya, S., Wadhwan, V., Kaur, G., Pathak, A. (2016) Seesaw of matrix metalloproteinases (MMPs). J. Cancer Res. Ther., 12(1), 28-35. DOI
- Laronha, H., Caldeira, J. (2020) Structure and function of human matrix metalloproteinases. Cells, 9(5), 1076. DOI
- Gialeli, C., Theocharis, A.D., Karamanos, N.K. (2011) Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J., 278(1), 16-27. DOI
- Bauvois, B. (2012) New facets of matrix metalloproteinases MMP-2 and MMP-9 as cell surface transducers: outside-in signaling and relationship to tumor progression. Biochem. Biophys. Acta, 1825(1), 29-36. DOI
- Dufour, A., Overall, C.M. (2013) Missing the target: matrix metalloproteinase antitargets in inflammation and cancer. Trends Pharm. Sci., 34(4), 233-242. DOI
- Melincovici, C.S., Boşca, A.B., Şuşman, S., Mărginean, M., Mihu, C., Istrate, M., Moldovan, I.M., Roman, A.L., Mihu, C.M. (2018) Vascular endothelial growth factor (VEGF) - key factor in normal and pathological angiogenesis. Rom. J. Morphol. Embryol., 59(2), 455-467.
- Karaman, S., Leppänen, V.M., Alitalo, K. (2018) Vascular endothelial growth factor signaling in development and disease. Development, 145(14), dev151019. DOI
- Roskoski, R.Jr. (2007) Vascular endothelial growth factor (VEGF) signaling in tumor progression. Crit. Rev. Oncol. Hematol., 62(3), 179-213. DOI
- Gao, F., Yang, C. (2020) Anti-VEGF/VEGFR2 monoclonal antibodies and their combinations with PD-1/PD-L1 inhibitors in clinic. Curr. Cancer Drug. Targets, 20(1), 3-18. DOI
- Schröpfer, A., Kammerer, U., Kapp, M., Dietl, J., Feix, S., Anacker, J. (2010) Expression pattern of matrix metalloproteinases in human gynecological cancer cell lines. BMC Cancer, 10, 553. DOI
- Sato, T., Sakaia, T., Noguchi, Y., Hirakawa, M.T.S., Ito, A. (2004) Tumor-stromal cell contact promotes invasion of human uterine cervical carcinoma cells by
- augmenting the expression and activation of stromal matrix
- metalloproteinases. Gynecol. Oncol., 92(1), 47-56. DOI
- Azevedo Martins, J.M., Rabelo-Santos, S.H., do Amaral Westin, M.C., Zeferino, L.C. (2020) Tumoral and stromal expression of MMP-2, MMP-9, MMP-14, TIMP-1, TIMP-2, and VEGF-A in cervical cancer patient survival: a competing risk analysis. BMC Cancer, 20(1), 660. DOI
- Rao, X., Huang, X., Zhou, Z., Lin, X. (2013) An improvement of the 2ˆ(-delta delta CT) method quantitative real-time polymerase chain reaction data analysis. Biostat. Bioinformfa. Biomath., 3(3), 71-85.
- Dabbs, D.J. (2006) Diagnostic Immunohistochemistry, 2nd ed. Elsevier, Philadelphia.
- Breznik, B., Motaln, H., Lah Turnšek, T. (2017) Proteases and cytokines as mediators of interactions between cancer and stromal cells in tumours. Biol. Chem. 398(7), 709-719. DOI
- Brown, G.T., Murray, G.I. (2015) Current mechanistic insights into the roles of matrix metalloproteinases in tumour invasion and metastasis. J. Pathol., 237(3), 273-281. DOI
- Qiao, Y., Wan, J., Zhou, L., Ma, W., Yang, Y., Luo, W., Yu, Z., Wang, H. (2018) Stimuli responsive nanother-apeutics for precision drug delivery and cancer therapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol., 11(1), e 1527. DOI
- Cun, X., Li, M., Wang, S., Wang, Y., Wang, J., Lu, Z., Yang, R., Tang, X., Zhang, Z., He, Q. (2018) A size switchable nanoplatform for targeting the tumor microenvironment and deep tumor penetration. Nanoscale, 10(21), 9935-9948. DOI
- Daniele, A., Abbate, I., Oakley, C., Casamassima, P., Savino, E., Casamassima, A., Sciortino, G., Fazio, V., Gadaleta-Caldarola, G., Catino, A., Giotta, F., De Luca, R., Divella, R. (2016) Clinical and prognostic role of matrix metalloproteinase-2, -9 and their inhibitors in breast cancer and liver diseases: A review. Int. J. Biochem. Cell. Biol., 77(Pt A), 91-101. DOI
- Kerbel, R.S. (2008) Tumor angiogenesis. N. Engl. J. Med., 358(19), 2039-2049. DOI
- Tewari, K.S., Sill, M.W., Long, H.J. 3rd, Penson, R.T., Huang, H., Ramondetta, L.M., Landrum, L.M., Oaknin, A., Reid, T.J., Leitao, M.M., Michael, H.E., Monk, B.J. (2014) Improved survival with bevacizumab in advanced cervical cancer. N. Engl. J. Med., 370(8), 734-743. DOI
- Solovуeva, N.I., Timoshenko, O.S., Gureeva, T.A., Kugaevskaya, E.V. (2015) Matrix metalloproteinases and their endogenous regulators in squamous cervical carcinoma (review of the own data). Biomeditsinskaya Khimiya, 61(6), 694-704. DOI
- Araújo, R.F. Jr., Lira, G.A., Vilaça, J.A., Guedes, H.G., Leitão, M.C., Lucena, H.F., Ramos, C.C. (2015) Prognostic and diagnostic implications of MMP-2, MMP-9, and VEGF-α expressions in colorectal cancer. Pathol. Res. Pract., 211(1), 71-77. DOI
- Zheng, H., Takahashi, H., Murai, Y., Cui, Z., Nomoto, K., Niwa, H., Tsuneyama, K., Takano, Y. (2006) Expressions of MMP-2, MMP-9 and VEGF are closely linked to growth, invasion, metastasis and angiogenesis of gastric carcinoma. Anticancer Res., 26(5A). 3579-3583. DOI
- Sawada, M., Oishi, T., Komatsu, H., Sato, S., Chikumi, J., Nonaka, M., Kudoh, A., Osaku, D., Harada, T. (2019) Serum vascular endothelial growth factor A and vascular endothelial growth factor receptor 2 as prognostic biomarkers for uterine cervical cancer. Int. J. Clin. Oncol., 24(12), 1612-1619. DOI
- Solovyeva, N.I., Timoshenko, O.S., Kugaevskaya, E.V., Andreeva, Yu.Yu., Zavalishina, L.E. (2014) Key enzymes of degradation and angiogenesis as factors of tumor progression for squamous cell cervical carcinoma. Russian Journal of Bioorganic Chemistry, 40(6), 688-696. DOI
- Brummer, O., Böhmer, G., Hollwitz, B., Flemming, P., Petry, K.U., Kühnle, H. (2002) MMP-1 and MMP-2 in the cervix uteri in different steps of malignant transformation - an immunohistochemical study. Gynecol. Oncol., 84(2), 222-227. DOI
- Wang, H.L., Zhou, P.Y., Zhang, Y., Liu, P. (2014) Relationships between abnormal MMP2 expression and prognosis in gastric cancer: a meta-analysis of cohort studies. Cancer Biother. Radiopharm., 29(4), 166-172. DOI
- Lu, X., Duan, L., Xie, H., Lu, X., Lu, D., Lu, D., Jiang, N., Chen, Y. (2016) Evaluation of MMP-9 and MMP-2 and their suppressor TIMP-1 and TIMP-2 in adenocarcinoma of esophagogastric junction. Onco. Targets Ther., 9, 4343-4349. DOI
- Fernandes, T., de Angelo-Andrade, L.A., Morais, S.S., Pinto, G.A., Chagas, C.A., Maria-Engler, S.S., Zeferino, L.C. (2008) Stromal cells play a role in cervical cancer progression mediated by MMP-2 protein. Eur. J. Gynaecol. Oncol., 29(4), 341-344.
- Mandic, A., Usaj Knezevic, S., Kapicl Ivkovic, T. (2014) Tissue expression of VEGF in cervical intraepithelial neoplasia and cervical cancer. J. BUON, 19(4), 958-64.
- Sawada M., Oishi T., Komatsu, H., Sato, S., Chikumi, J., Nonaka, M., Kudoh, A., Osaku D., Harada, T. (2019) Serum vascular endothelial growth factor A and vascular endothelial growth factor receptor 2 as prognostic biomarkers for uterine cervical cancer. Int. J. Clin. Oncol., 24(12), 1612-1619. DOI